By Megan Widdows
Antibiotics are drugs that are used to treat bacterial infections. Their discovery and development in the 20thcentury led to huge improvements in standards of living, healthcare and mortality from infection across the globe.
Before the discovery of antibiotics, our average life expectancy was just 47 years. The world was rife with infectious bacterial diseases such as smallpox, cholera, syphilis, tuberculosis and the plague and getting infected meant developing severe symptoms, with a high chance of dying.
This began to change with the discovery of penicillin, a key antibiotic, by Sir Alexander Fleming in 1928. It would take another 14 years for penicillin to be purified and produced on large enough scales to be used clinically, with its use originally restricted to the treatment of Allied soldiers in World War Two. Some historians argue that this likely contributed to their ultimate victory in 1945, allowing soldiers to recover from once deadly infections to fight another day.
Following the war, antibiotics soon became a widely available treatment, marking the start of the antibiotic era. During this time, scientists also discovered lots of other new antibiotics which helped to further revolutionise the treatment of infectious diseases worldwide. Unsurprisingly, this time saw major changes in the causes of death. In the US, for example, the leading cause of death switched from infectious diseases to non-communicable diseases such as cancer and cardiovascular disease whilst life expectancy jumped to 79 years.

Additionally, the impact of antibiotics was not limited to healthcare. They were, and still are, used widely in veterinary care and farming, not only to preserve the lives of livestock but also in soil management and crop production. This has led to increases in yields, and reduced costs for farmers as fewer animals are lost to infectious diseases.
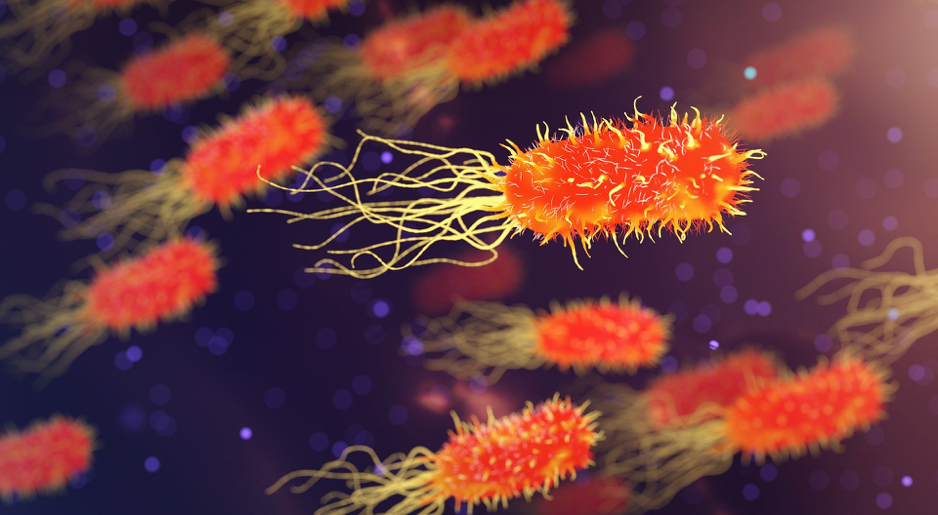
However, these improvements are threatened by the emergence of antibiotic resistance, which is the ability of bacteria to resist the effect of an antibiotic that they are usually sensitive to.
In nature, some bacteria are innately more resistant to antibiotics than others, so when antibiotics are used, these bacteria will survive whilst non-resistant species are wiped out. The survivors replicate and soon become the dominant species. Additionally, bacteria replicate, or reproduce, at extremely fast rates, which means mutationsare very common. Mutations are errors made during the DNA replication process, the result being an altered DNA sequence in the offspring. Sometimes these mutations cause a bacterium to become more resistant to the effect of an antibiotic, so it can survive treatment and continue to replicate. Resistance then becomes prevalent across the species.
The problem of resistance is exacerbated by the inappropriate use of antibiotics. Examples of inappropriate use are over-prescribing, especially for viral infections for which they are not effective; patients not taking the full course of antibiotics, giving more resistant bacteria a greater chance of survival; and their overuse in livestock and fish farming. Using antibiotics at sub-optimal doses is also thought to contribute to the development of resistance.
A lot of research has been devoted to studying the development and mechanisms of antibiotic resistance in a bid to find a solution and preserve the usefulness of antibiotics. However, research has rarely considered the impact that different antibiotic doses can have on the development of resistance. It is important to think about this when studying antibiotic resistance because antibiotics are used in varying concentrations, or doses, depending on the nature of the infection and who/what is being treated. Even when given the same dose, antibiotics are absorbed, processed and eliminated in different ways within the body of a treated animal or human, leading to a huge variation in doses. Some components of antibiotics can even diffuse over long distances, resulting in contamination of soils, water and other natural elements. This means there is an extremely wide spectrum of antibiotic doses within populations and our environment. But how does this effect the evolution of resistance?
We know that different environmental conditions lend themselves to distinct adaptations, where organisms evolve traits that make them better suited to their environment. Different concentrations of antibiotics produce different environments, which could mean bacteria evolve in different ways at different doses.

Scientists from the University of Montpellier in France set out to discover what effect different antibiotic doses may have on the evolution of resistance in bacteria. They found that, at all doses, the bacteria quickly adapted to become resistant. The higher the dose was, the faster this resistance evolved. This makes sense because at higher doses, there is a stronger selection pressure for resistant bacteria – bacteria that are not resistant will quickly be eliminated so that only the most resistant bacteria remain and can replicate.
The results also showed that, at different doses, the bacteria evolved to have distinctly different adaptations that conferred their resistance. Importantly, the adaptations for resistance at low doses, did not confer resistance at high doses and similarly, adaptations to high dosage did not protect bacteria at low doses.
This knowledge helps scientists to fully understand the way antibiotic resistance evolves, and affirms the importance of considering the effect of dosage on the development of resistance. This information will be essential in developing effective antibiotic resistance management strategies, hopefully enabling us to reap the benefits of antibiotics for years to come.
The study mentioned in this article can be found here. A glossary of key terms is provided below.
Tell us what you think about this blog…
We are trying to understand who reads our blogs and why, to help us improve their content.
By completing this survey, you agree that you are over the age of 18 and that your responses can be used in research at the University of Sheffield to evaluate the effect of blogging in science communication.
Glossary
Adaptations – the process of evolution that enables an organism or species to become better suited to their environment.
Antibiotic era – the period from the 1950s to present day, marked by the ability to effectively use antibiotics to fight bacterial infections. We are potentially facing an oncoming post-antibiotic era where antibiotics are no effective due to widespread resistance.
Antibiotic resistance – occurs when the bacteria develop adaptations that provide protection against antibiotics, meaning they are no longer killed by the same dose that used to eliminate an infection.
Mutations – changes to the structure or make up of a gene that can result in changes to an organism and/or its offspring
Selection pressure – an external factor that affects an organisms ability to survive in an given environment, adapting to this pressure increases chance of survival.
